Abstract
Objective:
Severe thalassemia syndromes (ST) are the most common non-infectious life-threatening disease in South Asia. ST is highly curable by BMT but rejection may occur in 5 to 30% of cases. In a limited resource setting appropriate case selection for BMT and aggressive down staging pre-transplant are crucial in order to achieve optimal outcomes. Though hepatomegaly > 2 cm has clearly been proven to be associated with poor transplant outcomes whereas the role of splenomegaly as an independent risk factor for rejection in low risk thalassemia has not been clarified.
Methods:
We analyzed a total of 87 consecutive first bone marrow transplants carried out between August 2013 and Dec 2016 after conditioning with busulfan (14 mg/kg oral, not adjusted to serum levels), cyclophosphamide (200 mg/kg) and anti-thymocyte globulin (Genzyme 4 mg/kg or Fresenius 16 mg/kg on days -12 to -10). 74 patients received cyclosporine and methotrexate, and 13 patients received cyclosporine and mycophenolate as GVHD/rejection prophylaxis. G-CSF-primed bone marrow (5 μg/kg/dose twice daily for 3 to 5 days prior to harvest) was the source of hematopoietic stem cells in all cases. All patients were considered low risk based on liver size < 2 cm from costal margin and age less than 15 years (median 6.9 years, range 1.1 to 14.5). All sibling couples were HLA-compatible.
Results:
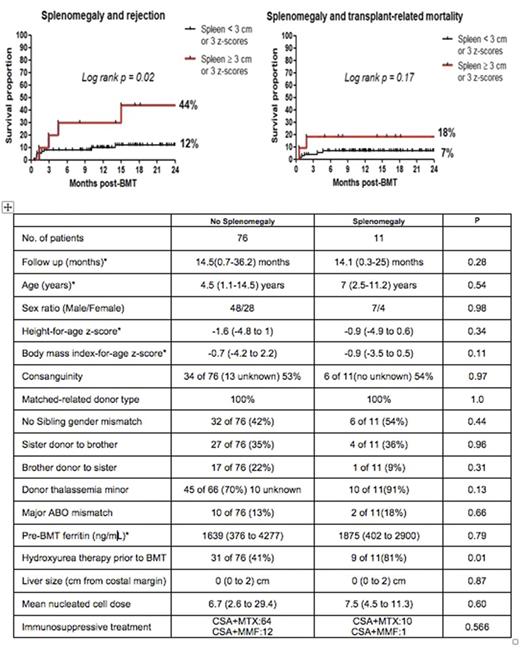
Of the 87 low risk transplants 12 children rejected (13.8%) of which 5 were primary and 7 were secondary graft failures. Out of the total 87 patients 11 patients had significant splenomegaly at transplant (spleen > 3 cm below costal margin and/or z score > 3 spleen size measured by ultrasound adjusted for height). Four of the rejections (1 primary and 3 secondary) occurred in children with significant splenomegaly which is statistically significant (log rank p=0.02) (figure 1). Splenomegaly also seems to increase treatment-related mortality albeit not statistically significant (log rank p=0.17). Out of the 7 children who had treatment related mortality 2 had splenomegaly. One of them died as a consequence of primary graft failure and the other due to a large intracranial bleed. We could not detect any difference in other variables potentially associated with rejection risk such as gender mismatch, serum ferritin, ABO mismatch, mean cell dose (median 6.75; range 2.6 to 29.44 x 108 nucleated cells /kg) and immunosuppressive therapy between splenomegaly and no splenomegaly groups. In the latter group 41% of children received hydroxyurea pre-BMT compared to 81% in the splenomegaly group (P= 0.01) which in fact should have helped to reduce rejection rates in the splenomegaly group. By multivariate analysis significant splenomegaly (p= 0.0049) seems to be more relevant than gender mismatch in terms of rejection risk (p = 0.0379), while cell dose (p=0.9546) was not a significant factor.
Conclusion:
Splenomegaly may increase rejection risk in low risk thalassemia transplants transplanted with ATG-BuCy. Strategies to reduce spleen size prior to transplant should be considered.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.